RANDOLPH, Vt.—The work by the Antibiotic Stewardship Committee at Gifford Medical Center to address antibiotic resistance, a continuing public health threat across the United States and globally, has resulted in a greater than 50 percent reduction in the use of the drugs with Gifford patients.
Overuse of antibiotics contributes to antibiotic resistance, the ability of bacteria to resist the effects of the medications that were once successful in treating them. According to a recent report by the Centers for Disease Control (CDC), “More than 2.8 million antibiotic-resistant infections occur in the U.S. each year, and more than 35,000 people die as a result.”
Gifford’s multidisciplinary Antibiotic Stewardship Committee includes physicians, pharmacists and infection prevention specialists. Over the last year and a half, the committee has developed protocols that have been implemented across the medical center’s inpatient units to reduce the number of antibiotics prescribed.
“We are attacking the issue of antibiotic resistance from various angles, and have cut the number of antibiotics we’re using with our patients by more than half,” said Gifford Chief Medical Officer Dr. Joshua White.
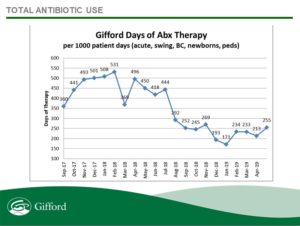
White shared data indicating Gifford inpatient days of antibiotics therapy from September 2017 through April 2019. Comparing April 2018 with April 2019, for example, per 1,000 patient days, Gifford usage dipped from 496 days of antibiotics therapy to 213 days.
The Antibiotic Stewardship Committee’s initiatives include a 72-hour antibiotic timeout, in which antibiotics are stopped during inpatient rounds to review whether they are still needed and whether the medication is the appropriate antibiotic; Gifford-specific adult and pediatric quick reference guides for clinic and Emergency Department providers; and increased provider education, including review of stewardship efforts and reports at medical division meetings.
In addition, Gifford has implemented a procalcitonin (PCT) testing strategy to evaluate the use of antibiotics in lower-respiratory infections. The test can be helpful in determining whether antibiotics should be used, as high levels of PCT indicate a bacterial infection while low levels indicate a viral infection or other cause.
“Overuse of antibiotics for lower respiratory tract infections,” according to a study published by the National Institutes of Health (NIH), “is one of the most urgent and difficult stewardship problems in U.S. hospitals, accounting for much of the unnecessary antibiotic use in the inpatient setting.”
Gifford’s antibiotic stewardship is bucking national trends, said White. He referred to the rise of quinolone-resistant E. coli in the U.S. Quinolones are a class of antibiotics.
“For the second year in a row, we have seen an increase in quinolone sensitivity of E. coli in our urine studies – the exact opposite of what is happening on the national stage,” said White.
For more information about antibiotic resistance, visit cdc.gov.
# # #
Gifford is a community hospital in Randolph, Vt., with family health centers in Berlin, Bethel, Chelsea, Randolph, Rochester, and White River Junction; and specialty services throughout central Vermont. A Federally Qualified Health Center and a Top 100 Critical Access Hospital in the country, Gifford is a full-service hospital with a 24-hour emergency department and inpatient unit; many surgical services; a day care; two adult day programs; and the 30-bed Menig Nursing Home, which was named by U.S. News & World Report as one of the best 39 nursing homes in the country in 2012. The Birthing Center, established in 1977, was the first in Vermont to offer an alternative to traditional hospital-based deliveries, and continues to be a leader in midwifery and family-centered care. The hospital’s mission is to improve individuals’ and community health by providing and assuring access to affordable, high-quality health care in Gifford’s service area.

