Mindi was taking a nighttime walk near her Vermont home when Minnow, her affectionate golden retriever, bounded into her from the opposite direction. It was dark, Minnow was enthusiastic, and Mindi fell. She ended up with a fractured tibial plateau, a break at the upper part of the shinbone at her knee, and unable to walk.
Mindi required surgery to repair the fracture and now, 11 weeks after the procedure, she can be found teaching her body to walk again with the help of the Physical Therapy (PT) team at Twin River Health Center. Since mid-January she’s been doing two sessions a week, one at Twin River’s downtown White River Junction location and the other in the pool at Upper Valley Aquatic Center.

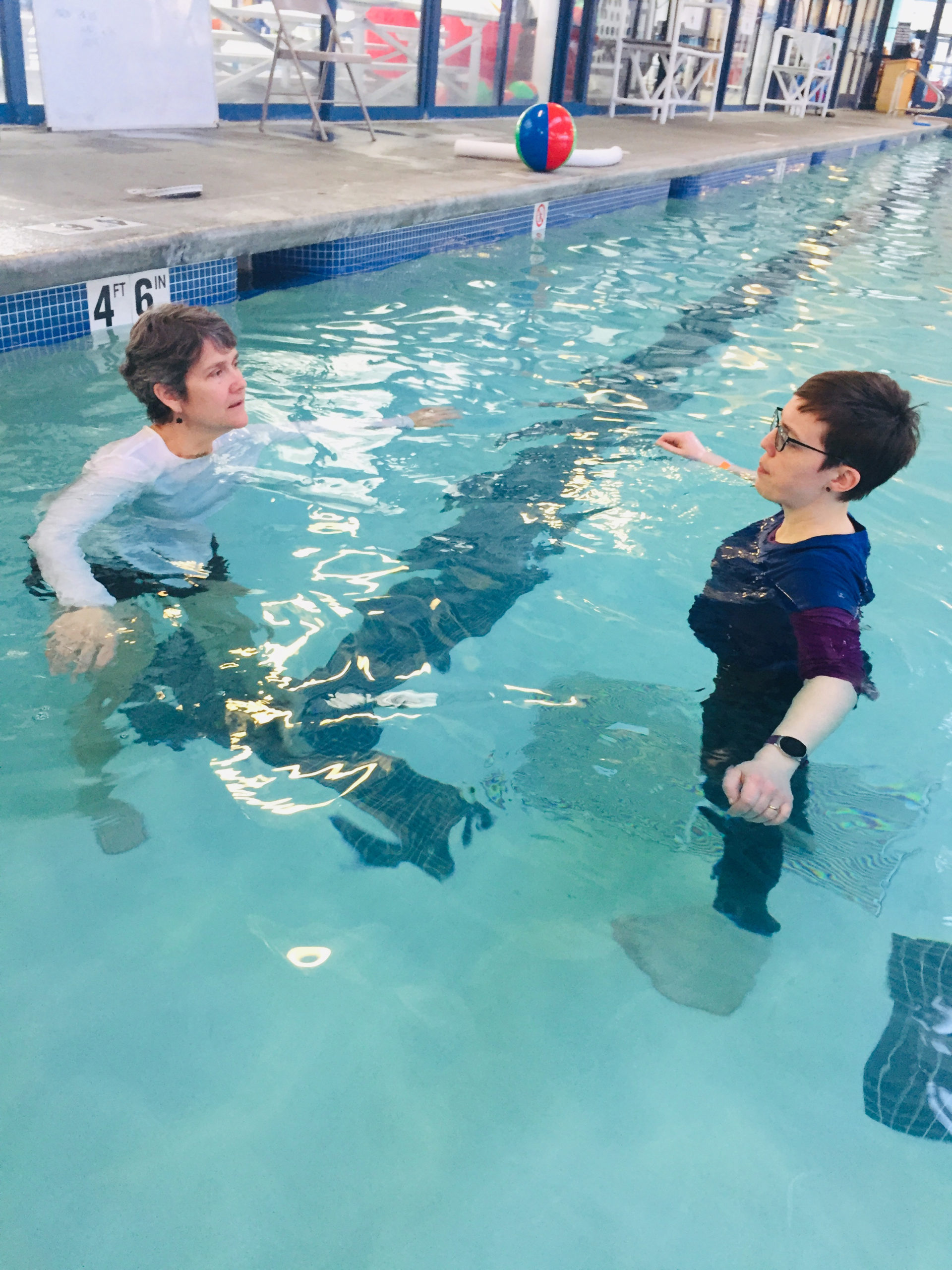
Mindi, left, and Gifford PT Assistant Jo work in the pool at Upper Valley Aquatic Center in White River Junction, VT.
“When I was talking to my doctors after surgery, I asked about [aquatic] therapy because it sounded like it was something I could do without worrying about falling, where I’d feel safe,” Mindi said of her proactive approach to rehabilitation during a recent poolside interview. “Every time you move in water your body benefits from it. They said it was a great idea.”
Mindi had clear goals for PT.
“I wanted to start walking again, to rebuild the muscle I lost, to retrain my body,” she said. “I needed to get my range of motion back, and get back to where I was before I was injured.”
Physical Therapist Amy Chiriatti works with Mindi on land and coordinates care with PT Assistant Jo Alexander, who provides therapy in the pool. Together they are helping Mindi achieve her goals.
Today, “I’m feeling much stronger,” Mindi said. “My range of motion and muscle have improved enormously. I can fully straighten my leg and can bend it beyond 120 degrees. I am walking with one crutch now as well. I couldn’t do any of those things a few weeks ago.”
While she continues to see her doctors every four to six weeks, Mindi credits the PT team for accelerating her rehabilitation.
“It’s a very different experience working with the physical therapists,” she said. “They get me through the day-to-day stuff. They are both awesome and very encouraging. Just working with anyone in PT is reassuring, because they’ve worked with other people who have gone through this.”
“What I appreciate most about working with Amy and Jo is how knowledgeable, supportive, reassuring and encouraging they are. I guess that’s four things!”
Q&A with PT
Here, Amy and Jo answer questions about their plan of care for Mindi, outpatient physical therapy and benefits, and what patients can expect:
How do you work together to achieve Mindi’s goals? How do you tailor your sessions to complement what the other is doing?
Amy: Mindi is a prime example of the perfect pool/rehab patient. She has been using the pool for gaining confidence in walking and learning the correct stepping patterns, because she was non-weight bearing for so long. She also needs land for manual therapy to work on range of motion, and strength exercises that she can do at home on her own.
After we evaluate a patient and think water therapy will be helpful, we schedule them for the pool. I write in my plan of care what general strategies I would like to use, like strengthening or balance. Strengthening can be land- or pool-based, so Jo has a place to start her program. Under a physical therapist’s supervision, Jo modifies the activities to best suit the patient (that patient on that day). She takes everything into account: their condition, their comfort with water, the surrounding activities, their pain levels, and their functional abilities. If a patient responds poorly, or better than Jo expected, she modifies her plan to their needs.
Jo, as the PT assistant, and the referring PT are always communicating about our patients and concerns or progression or status changes. We have time built into our schedule for these meetings. Also, our daily progress notes communicate our treatments and our patient’s responses. These notes give anyone on our team an idea of where to work next and how the patient is responding.
Jo: When we both work with a patient in the clinic, I often follow very closely what Amy does with them, but with my own perspective, or if they have multiple things to work on, she might focus in one area on a Thursday, and I focus on the other on a Monday. When I’m in the pool with a patient, I focus on the activities that are hardest or impossible to do on land – like going up steps, or gaining core strength or balance.
Why, and for whom, is PT important?
Amy: Oh, let me count the ways! I can find something to work on in nearly anyone. Almost everyone needs to work on posture. Older people almost always need to work on balance and strength. But, because their declines are so gradual, they don’t register as changes. PT can be helpful to jump-start healing, to learn or relearn a skill or task. PT also works on functional gains, like reaching into a cupboard, standing from a chair, climbing stairs, rolling over in bed, or donning a sock.
Jo: PT can help a huge variety of issues, from balance and other neurological challenges to recovery from muscle, tendon, or bone injury or surgery.
Mindi shared that her goals are to retrain her body to walk, to rebuild muscle she lost, and to get range of motion back to where she was before she was injured. What other types of goals do you help patients set and achieve?
Amy: Our goals are designed to reflect what the patient wants to do. Sometimes they are functional, maybe based on activities of daily living, like brushing hair, standing to make dinner, getting into the car. Other goals are for fitness and activity tolerance – play a full game of soccer, run a half-mile without foot pain, lose weight before a knee replacement. Objective measurements help document progress toward those goals. For example, you need 110 degrees of knee bend to sit in a normal chair or toilet. You need 115 degrees of arm elevation to do your hair, and 52 degrees to wash your armpit.
Why aquatic physical therapy? What are the benefits?
Amy: I think aquatics is particularly helpful when people are recovering from an injury or surgery and are remembering how to walk properly. It is very important to transition from non-weight bearing to stepping onto your sore foot/leg with the correct gait pattern. It is much easier to get it right with therapy than to try to correct it if it is learned poorly. Aquatics is beneficial for recovering from ankle sprains, fractures, surgical pinning, knee replacements, hip replacements.
Jo is also brilliant in the pool when patients need work on shoulder rehab. Water is a great modality to use as much or as little resistance as is needed/wanted. Arms float, so water easily helps range of motion. Buoyancy is a key factor to water therapy. It reduces weight bearing through the whole body, so people with back pain also experience less downward compressive force on their spines. Also, the “inward” pressure is helpful for edema (or lymphedema) swelling, and painful joints. People find it easier to get range of motion after surgeries when they work in the water. And people with muscle spasms or spasticity, as in cerebral palsy, find the water calming, and the pain and tension from the muscles can be reduced.
We like to get the surgical cases in the water as soon as their scar is healthy and closed fully. We have access to a lift chair, so if someone has difficulty with stairs, there is an alternative way to get in the pool. Water is a great tool to work on balance issues. The light perturbation from water waves can challenge the balance nicely. The lazy river at the pool has been a big favorite for rehab. It is fun to let the water float you around, and for advanced rehab, you might be asked to walk against the current.
Often when we have a patient that is right for the pool, we also want to have land therapy, in which case Jo and I will each see them in a week’s time. Some patients need more aggressive pool therapy than land therapy, but they will be scheduled to see a physical therapist every few visits to assess changes and make sure the goals are still appropriate.
Jo: One great thing about getting into the pool is that a person who has weight-bearing limits due to surgery can still exercise, and if they are allowed to bear weight a little, we can start that process in the water.
The pool is perfect for anyone who has difficulty exercising on land due to pain, being overweight, balance issues, or difficulty walking due to surgery or injury. Pool exercise also can be a great way for athletes to cross-train with less impact!
What can a patient expect during their first PT session? How do you begin?
Amy: In the first session, we evaluate the patient, generally find a therapeutic exercise or two to help the situation, and hopefully find a way to ease the pain or other condition. We begin with a verbal interview. We find out how long they’ve been dealing with their condition, how it may have started, what they maybe did to help themselves, pain level, what they have difficulty doing because of their situation, and what they might like to get out of therapy.
Then, we move into the physical part of the evaluation, hoping to pinpoint the root cause of the problem, or confirm the given diagnoses. We gather measurements which help us work toward specific goals. This might be range of motion, strength, activity tolerance, ability to climb stairs (functional strength), or balance. We perform specific tests to isolate various tissues to differentially diagnose the condition. For example, rotator cuff tear versus tendonosis, versus shoulder impingement. Or meniscus tear, ligament sprain, patella-femoral syndrome; or back strain versus herniated disc. Pain and symptoms are sometimes really hard for people to describe, so by loading a tissue, possibly reproducing the symptom, we can better know what the problem is and how to treat it.
All therapist have different interests and techniques, but I like to do some manual therapy, which often makes an immediate difference in pain levels, and give an exercise so they can start working on their own and taking care of themselves. Other therapists prefer a hands-off approach, believing the less they do, the more the patient will work for themselves.
A big part of my job is patient education. I pull out my anatomy book or walk them over to the skeleton so they can see what “normal” looks like, then I tell them what is different about my findings. I try and give them an idea of our general plan of care, and what they can expect. I try to give them ideas of healing times. I walk them to the front desk, ask them to schedule follow-ups based on my findings and the plan of care. I print out or draw their exercises or tasks for the next week or so. And I ask if they have any further questions.
In terms of pool referrals, sometimes I get to that in the first session. Sometimes I don’t have time, or want to get to know the patient better before I spring on another treatment type. When I’ve gathered this info, I chat with Jo and we come up with a plan.
How do you determine how long PT lasts?
Amy: PT episodes will usually last until the patient has met their goals. If I were to guess an average, I might say six to eight weeks. But PT services have changed in the last 20 years. It is much less likely that you’ll be able to see a patient in an outpatient setting three times per week, like it used to be. More commonly, it’s twice a week, max.
With our demographics in the Upper Valley, our patients want to be more independent and seem to want to come to PT as little as possible. There are work and time constraints, insurance costs, gas costs and other transportation issues. But I’d say that most people just want to do more on their own. If a patient has stopped making progress, that’s a reason to reconsider the benefits of PT and maybe stop. And if a patient has a significant change in condition, we might end PT before the goals are met.
How do you coordinate care with a patient’s physician and/or other members of their health care team?
Amy: Generally we get a referral from a primary care provider (PCP) for a specific diagnosis, and we work on that. Vermont has Direct Access*, so patients can come to PT directly without first seeing a PCP, but their insurance might suggest otherwise. If a patient is post-surgical, or planning on seeing their doctor again, we’ll write a progress note and send it over so the doc has a heads-up about what is going on, what changes have happened, etc. If we have any questions about care for the patient, we call the doctor’s office. Most doctors are really good about getting information back to us. They also want their patients to succeed.
What inspired you to work in physical therapy? Why did you choose this line of work?
Amy: What cinched the deal for me, years after I earned my bachelor’s, was when I was working as a personal caregiver for a 42-year-old woman with cerebral palsy. She was bound to a motorized wheelchair. Eventually I asked her if she’d let me walk with her. When I walked her the length of her apartment, I was in love. I don’t do that kind of work now, but that walk was the tipping point for me to tick off my prerequisites and apply for grad school to pursue physical therapy.
Jo: I had a few injuries from running and martial arts that benefited significantly from physical therapy, and my friend Amy Chiriatti, now my co-worker, recommended I become a PT assistant due to my interest in the field. Thanks, Amy!
#
*Direct Access
Per Vermont law, a physician referral is not required for a physical therapist to evaluate or treat a patient, and there are no provisions to treatment. Patients can go directly to physical therapy without a referral from their PCP or specialist. Many insurance programs allow this, but a patient should be sure to check their individual plan as all plans are different.
“Direct Access has been found to save people money and provides a more efficient path for patients to improve their health,” said Gifford Rehabilitation Services Manager Troy Stratton, citing a study on the cost-effectiveness of Direct Access to PT. “And if therapists don’t see progress within the first few visits, they can refer the patient back to their PCP if needed.”
#
For more information about PT and other rehabilitation services at Gifford, visit giffordhealthcare.org/service/rehabilitation.
###



