By Dr. Josh White
Gifford Chief Medical Officer
The only thing we have to fear is fear itself.
-FDR
Reflection on the early days of the pandemic is an interesting exercise. A short two years ago feels like a lifetime, and yet fear of the unknown still freshly lingers. We aren’t that far from the lockdowns, the overflowing hospitals in Italy and NYC, or the refrigerator trucks converted to makeshift morgues. The anxiety amongst our neighbors is easy to understand.
Yet, the reality is that things are different now. Omicron is not Delta and Delta was not Alpha. We are, in effect, dealing with a different virus. As such, policies and attitudes need to be revisited. Living with Covid-19 is now the goal, not hiding from it, nor pretending it will go away. It is time to let go of our anxiety.
Omicron came to us like a brush-fire, more infectious than previous variants. Despite the discomfort that statement might provoke, this appears to be a blessing in disguise. A recent study of Southern Californians with the omicron variant of SARS-COV-2 concluded that, “SARS-CoV-2 infections with presumed Omicron variant infection were associated with substantially reduced risk of severe clinical endpoints and shorter durations of hospital stay.” In other words, out of 52,297 patients, only 0.5% were hospitalized and none of these patients received mechanical ventilation. Omicron, particularly to the healthy and the vaccinated is not really very dangerous. And after an individual has been infected, they have antibodies and a relative degree of protection for the future.
Examining this from a different perspective, let us consider relative risk. Think about heart disease. Do you consider the threat of Covid-19 to be a greater or lesser threat than heart disease? Were you aware that heart disease killed more Americans in 2021 than Covid-19 in every single age group (and much of this data reflects the more severe delta variant)?
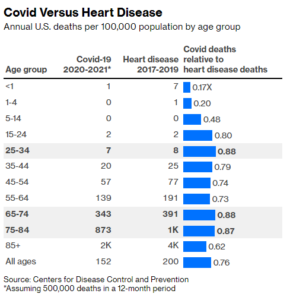
Does heart disease change the way we interact at work? Does it change the way our children go to school, interact with family, wear masks, or cause us all to behave differently every single day? To be intellectually consistent, it should. If we are changing our behavior for fear of Covid-19, we should be changing our behavior for fear of heart disease.
I am well aware that this may be shocking for some of you to read, and obviously, predicting the future is an imperfect game. But as we used science to direct us in the beginning and middle of the pandemic, we can use science to steer us to the end. We need not respond from a position of fear.
Keep in mind I am not suggesting we can forget about Covid-19, or that there is no burden. Are people dying from the Omicron variant? Certainly. The unvaccinated and the immunosuppressed remain at risk. Hospitalizations are still high, given the large spike in total cases. After all, a small percentage of a lot is still…a lot. But those numbers are coming down sharply. Covid-19 or not, healthcare systems are going to continue to struggle given workforce challenges. The unvaccinated and the immunocompromised will still have to be careful and in the future, people will die from Covid-19 in towns every year, much like influenza.
Returning to my original premise, we are largely exiting the proverbial woods. Why can I make such a claim?
- Data on Omicron is clear. This is a much milder disease.
- We have highly effective home antigen tests. Self-diagnosis and management of Covid-19 has become relatively easy.
- We now understand what this virus is, how it tends to behave, when to worry and when to relax. SARS-COV-2 is no longer an unknown.
- A very large percentage of the U.S. is now walking around with antibodies to SARS-COV-2, either through vaccination, Covid-19 infection, or both. We are not going to see another giant spike in cases.
- Although immunity may fade to a degree, repeat illness tends to be mild. Repeat illness also does not tend to precipitate long-Covid, lessening the disease burden. Although a future variant may push out Omicron, that scenario is becoming increasingly less likely. Variants become dominant based on how infectious they are. Once a variant has reached a point where it has infected most of the population all at once, there becomes less and less room for new variants.
- The pharmaceutical industry can now react with incredible speed. Pfizer has announced that it now has the capacity to develop a new vaccine within 100 days. Should a new variant of concern develop, the response will be immediate.
- We now have highly effective treatments for Covid-19. Paxlovid, an antiviral developed by Pfizer, is becoming increasingly available and has demonstrated an 89% reduction in hospitalization rates. Because Paxlovid is a protease inhibitor, it is relatively immune to the typical SARS-COV-2 mutations we have seen thus far. Paxlovid is likely to work just as well against any future variant.
- Simultaneously, monoclonal antibodies against any given variant can now be developed quite quickly. Even for the high risk and vulnerable amongst us, SARS-COV-2 is becoming less and less dangerous.
To make a long story short, we are not going back to 2019. We have made a lot of gains that are going to stay with us. We are going to be ok.